Did underfunding cause the winter crisis on the NHS?
SUGGESTED



I didn’t know the answer. There certainly weren’t any when I lived there: I had never heard that expression (or any synonym thereof) before I moved to the UK, just over a decade ago. But I haven’t followed it closely since then, and a lot can change in a decade, especially against the backdrop of demographic change, changes in morbidity patterns etc. So I searched Winterkrise [winter crisis], Krankenhauskrise [hospital crisis] and a few related search terms on the news section of Google.de, which would also have picked up media coverage of such a crisis in the Austrian and/or the Swiss health system, had there been one.
The first few entries were about the NHS winter crisis here in Britain (see e.g. here and here). Most were about the ‘winter crises’ of football clubs, where ‘winter crisis’ meant that they had lost a string of matches in winter. A few were about historical issues, namely the so-called hunger winter of 1947, and the stalled Wehrmacht attack on the Soviet Union in 1941/42. The only articles that were actually about healthcare in one of the German-speaking countries talked about the long-term (as opposed to acute) challenges that virtually every health system in the developed world faces. But nothing on a specific ‘winter crisis’ in any of those systems.
So no, winter crises are not inevitable. Why do we have them, when other countries (and the German-speaking countries aren’t exactly famous for their mild winters) don’t?
On social media, the matter is already settled: It is all just because of underfunding. Fund the NHS adequately, and it will be second to none.
At first sight, this seems to contain a grain of truth. We spend just under 10% of GDP on healthcare (mostly on the NHS, plus a bit of private spending). By international standards, that is not a lot. Most countries in North-western European spend between 10.4% and 12.4%. Thus, there is scope for extra healthcare spending in the UK, and it would almost certainly lead to some improvements.
Total healthcare spending in % of GDP, 2016
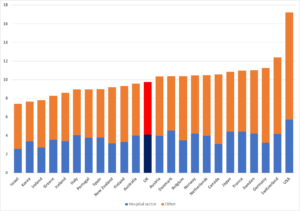
-Based on OECD (2018)
But overall healthcare spending is a huge aggregate. It includes GP services, pharmaceuticals, diagnostic tests, medical implants, medical devices, convalescent homes, a vast range of specialties, a vast range of hospital procedures, and so on. To say that differences in this massive aggregate are to blame for differences in one quite specific outcome is a bit of a leap of faith.
Suppose you travelled to Belgium, went for a pint, and really liked the beer. What would you make of it if somebody told you: “Of course you like it. As a percentage of GDP, Belgium spends more on beverages than we do. So that beer must be better than a British equivalent.” Not convincing, is it?
Once we break this massive aggregate down just a little bit, we get a rather different impression. Spending on the hospital sector (and the ‘winter crisis’ is really a hospital crisis) amounts to 4.1% of UK GDP. That is a completely normal figure by North-Western European standards.
In contrast, France and Germany spend over 2% of GDP on medical goods, compared to just around 1% in the UK. Maybe we would be better off if we increased spending in that category to their levels. Maybe it would improve people’s quality of life by enough to justify the extra cost. But it would not solve the winter crisis in the NHS.
People who blame the winter crisis on a lack of money seem to assume that if healthcare spending were increased by, say, 10%, this increase would be distributed evenly across all the different subsectors of the health sector. We would spend 10% more on nurses, 10% more on doctors, 10% more on syringes, 10% more on prescription drugs, 10% more on hospital beds, and so on.
This is not true. Healthcare spending is allocated according to clinical priorities. Crudely put, you spend the first few pounds on conditions that are matters of life or death. If you then still have money left, you spend it on conditions that are not immediately life-threatening, but that might well become so. If you then still have money left, you spend it on conditions that are not life-threatening and will not become so, but that are still seriously debilitating. If you then still have money left, you spend it on conditions that are not seriously debilitating, but still very unpleasant. If you then still have money left, you spend it on conditions that are not very unpleasant, but… you get the idea. The last few pounds are spent on the conditions with the lowest clinical priority.
Put differently, if a reasonably well-off person made an extra £100 per year, they might spend it on dining out or on wine. But it would probably not buy them better bread, better butter or better eggs.
Similarly, by and large, an increase in funding makes a health system more generous, but it does not automatically make it better at dealing with its core function.
The winter crisis is a bread-and-butter crisis. The problem is not that the system is not generous enough (although that may be a problem too, but it is not the problem which is generating headlines right now), but that it is not fulfilling its core functions well. Which suggests that the system is suffering from problems that money alone could not cure.
- Recommended reading: ‘Universal healthcare without the NHS‘ by Kristian Niemietz
4 thoughts on “Did underfunding cause the winter crisis on the NHS?”
Comments are closed.





One answer which never gets mentioned by those virtue signalling Doctors on Twitter is wages. Wages in the NHS, for Doctors, are very high compared to Europe, that’s why so many European Doctors come here. If you pay Doctors less, there is more money for other things.
unhelpful review of problems.
Hospital sector not the only issue – also need to look at social care.
For reference I suggest you compare hospital beds, nurses and doctors per 1000 population across different European countries.
And as for the comment above: genius. We are short of doctors (by any measure: unfilled posts, European average, etc). Let’s pay them less. Bound to sort out the problem.
Did I suggest we should pay them less? I did not, I was referring to European healthcare systems which do pay less and therefore have more money to spend elsewhere.
Surely the doctors who ‘love our NHS’ will be happy with a 10-15% pay cut to support ‘the envy of the world’ and support funding levels which are appropriate when compared to Europe? Are British Doctors worth their excessive pay? Their results, when compared to European results, appear to suggest they are not. Surely less pay, an equal society and more money for the NHS is favoured by the left?
You cannot be suggesting that Doctors will put pay before patients? It’s almost as if you are portraying them as virtue signaling, rent-seeking lefties expecting other people to pay and not really bothered about the NHS at all?
I agree 100% with Josh B, very unhelpful and uninformed politically motivated comments. There are two major issues in our Emergency departments. Firstly, the number of frail elderly patients arriving. The failure to properly fund social care for these patients, both in their own homes and in care homes, means that more of them turn up in ED needing admission and a long stay. Secondly, reducing the funding for social care and the resultant failure to provide adequate capacity in step-down care outside of hospitals means that we cannot discharge these patients in a timely way. Hence no beds available, hence patients backing up in ED. Try plotting these decreases in funding over the last few years against the volume of patients in ED and guess what, you will see a direct correlation. Austerity is a political choice made by this government, and the constant beasting of the NHS is designed to whittle away at the public’s rightly held affection for it. The aim of this is to drive healthcare into the private sector where profit-driven organisations will cherry-pick their patients and leave the rest – the poor, the sick, the terminally ill, those with multi-morbidities – to be dealt with by an underfunded rump of the NHS. Your paymasters’ beloved ‘free market’ only works for those at the higher end of the food chain.